Does Hunger Cause Ulcer?
13 mins,


You must have heard that skipping breakfast or not eating when you should are the reasons for your stomach ulcer. For a long time, people have associated ulcer with not eating, but does hunger cause ulcer?

“Mummy, I’m hungry but there’s this pain I feel, it’s like something is burning in my tummy”, Deji said amidst tears as he held his stomach.
“I’ve always told you to stop skipping your meals. I’m sure you’ve given yourself an ulcer. Let me consult Dr Angela on KompleteCare now to seek professional help.”
[Few minutes later, Deji’s mom hops on a quick video call with Dr Angela].
“Hello Doc, Please my son complained of severe pains when he was hungry. I suspect he has a stomach ulcer. He’s a very picky eater and always skips his meals.”
“Calm down mummy Deji. He will have to run some tests for us to ascertain that he really has a stomach ulcer. But to get relief from the stomach pain, I’ll write a prescription for him now.
“But Dr. Angela, does hunger cause ulcer?”
In this article, we’d share Dr Angela’s answer to Mummy Deji’s question, “Does hunger cause ulcers?”
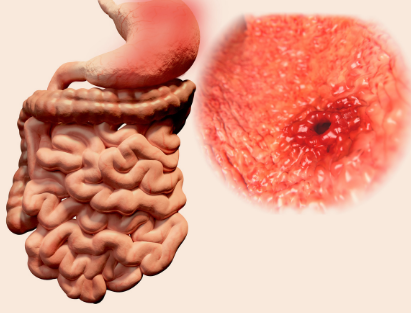
A stomach ulcer is a sore that forms on the inside lining of the stomach.
What really happens?
Your stomach is coated with a mucous layer that normally protects against digestive acid. This barrier is maintained by a balance between factors that promote mucosal defense (e.g., mucus, bicarbonate secretion, adequate blood flow) and factors that cause mucosal damage (e.g., gastric acid, pepsin, and bile salts).
Ulcers form when this balance is tampered with, leading to the erosion of the stomach lining by gastric acid and digestive enzymes.
Stomach ulcers may be easily cured, but they can become severe without proper treatment.
Stomach ulcers have a variety of symptoms, and their severity depends on how advanced the ulcer is.
The most common symptom is a burning sensation or pain in the middle of the tummy between the chest and belly button. This pain is usually more intense when the stomach is empty and can last from a few minutes to several hours. This experience, similar to hunger, often raises the question: does hunger cause ulcers?
Other common signs and symptoms of ulcers include:
– Dull stomach pain
– Weight loss
– Avoiding food due to pain
– Nausea or vomiting
– Bloating
– Feeling full quickly
– Heartburn, a burning sensation in the chest
– Pain that may improve with eating, drinking, or taking antacids
– Anaemia, with symptoms like tiredness, shortness of breath, or pale skin
– Dark, tarry stools
– Vomit that is bloody or looks like coffee grounds
Now you know the common symptoms of stomach ulcer, let’s find out the relationship between hunger and ulcer.

Just like identical twins, Hunger and ulcer can be similar but are different.
Hunger is a term used to describe the body’s cry for food, while ulcer occurs when the lining of the stomach is eroded by digestive acids.
Prolonged hunger, or fasting, can have several physiological effects on the body that influence the development of stomach ulcers:
1. Increased Gastric Acid Secretion:
During long periods without food, the stomach continues to secrete gastric acid, which can erode the stomach lining if not neutralized by food. This increased acid production can damage the mucosal lining of the stomach, potentially leading to the formation of ulcers.
2. Impaired Mucosal Protection:
Your stomach’s mucosal barrier relies on a regular supply of nutrients to maintain its job. Prolonged fasting can reduce the production of mucus and bicarbonate, which protect the stomach lining from acid and without adequate protection, the stomach lining becomes more prone to damage from gastric acids, increasing the risk of ulcer formation.
3. Stress:
Staying hungry for a long period of time can induce a stress response, leading to the release of cortisol and other stress hormones. These hormones can increase gastric acid production and decrease blood flow to the stomach lining, impairing its ability to repair itself.
The combination of increased acid and reduced mucosal defense can create conditions conducive to ulcer development.
Therefore, long periods of exposure to gastric acid can further damage the mucosal lining and contribute to ulcer formation.
Although Hunger is not the causative organism for ulcer, hunger can create the environment for ulcer to thrive which means that Yes! Hunger can cause ulcers.
Hunger is regulated by a complex combination of hormonal signals, neural pathways, and nutrient sensing mechanisms.
The following are important facts to note about hunger and how it occurs.
1. Hormonal Regulation:
Ghrelin, often called the “hunger hormone,” is produced in the stomach and stimulates appetite. This hormone is responsible for telling the brain to induce hunger. Ghrelin levels increase before meals and decrease after eating.
2. Glucose Levels:
Blood glucose levels are closely monitored by the body. When glucose levels drop, the liver signals the brain to induce hunger, prompting more consumption of food to boost energy levels
3. Stretch Receptors: The stomach and intestines contain stretch receptors that signal fullness or hunger based on the volume of food present.
This simply means that an empty stomach stimulates hunger signals, while a full stomach suppresses them.

There are two major causes of stomach ulcers:
NSAIDs, such as aspirin, ibuprofen, and naproxen, are medications commonly used for pain relief and inflammation. High doses of these medications can irritate the stomach lining and reduce the production of prostaglandins, which are substances that help maintain the stomach’s protective mucus barrier. This action increases the risk of ulcer formation.
Other causes of stomach ulcers include:
Smoking: Smoking increases stomach acid production and reduces the production of bicarbonate, which neutralizes stomach acid. It also stops blood flow to the stomach lining, delaying the healing process.
Alcohol Consumption: Excessive alcohol intake can irritate and erode the stomach lining, increasing acid production and making the stomach more vulnerable to damage from digestive juices.
Certain medical conditions can increase the risk of developing stomach ulcers. For example, Crohn’s disease and liver cirrhosis.
While Crohn’s disease is an inflammatory bowel disease that affects any part of the gastrointestinal tract, including the stomach, leading to ulceration, liver cirrhosis is a chronic liver disease leading to hypertension, which is associated with an increased risk of developing peptic ulcers.
READ ALSO:
■ Nigerian Food timetable for ulcer patients
Technically, at this point, it’s okay to say that gastric juice plays an important role in the stomach.
But the stomach has several ways to protect its lining from gastric acid. The stomach produces a thick mucus layer that traps bicarbonate, which helps counterbalance the acid.
This lining also renews itself quickly, with new cells replacing damaged ones. Prostaglandins help by increasing mucus and bicarbonate production and improving blood flow to the stomach lining, which aids in repair.
Also, tight junctions between epithelial cells prevent harmful substances from passing through. After eating, the stomach releases bicarbonate into the bloodstream, helping to neutralize any acid that gets through the mucus.
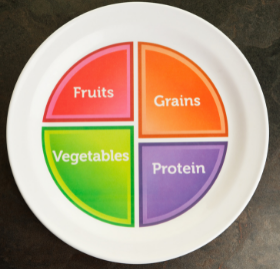
1. Buffering Effect:
Eating food acts as a buffer, balancing stomach acid and reducing its corrosive effects on the mucosal lining. This helps to prevent acid-related damage during digestion.
2. Stimulation of Protective Mechanisms:
Eating stimulates the production of mucus and bicarbonate, which are crucial for protecting the stomach lining. The presence of food prompts the stomach to enhance these protective secretions.
3. Prevention of Overproduction of Acid:
Consistent eating patterns help regulate acid production. Irregular eating or prolonged fasting can lead to increased acid production, which can overwhelm the stomach’s protective mechanisms and increase the risk of ulcers and other gastric issues.
The mucosal barrier protects the stomach lining from acid. It includes a thick mucus layer that traps bicarbonate, forming a shield against acid and damage. Bicarbonate suppresses the acid, keeping the stomach surface safe. The stomach lining cells renew quickly, replacing any damaged cells. Prostaglandins help by increasing mucus and bicarbonate and boosting blood flow to the stomach lining.

In addition to getting medications from a certified doctor, there are some actions you can take at home that can help in the treatment of your stomach ulcer.

With Telemedicine, there’s no distance in healthcare. Just like Deji’s mom reached out to Dr. Angela and got the help they needed, you too can have easy and fast access to expert doctors from the comfort of your home.
This means whenever you feel any discomfort or have a health concern, instead of self-medicating, speak to a doctor on KompleteCare to get prompt and quality medical attention that you deserve.
The fastest way to cure a stomach ulcer is to identify and treat the cause. The sooner you start antibiotics and other treatments, the sooner your ulcer will heal.
The most common cause of ulcers is infection by Helicobacter pylori bacteria, which are found in most people with peptic ulcers.
Long fasting periods can cause health issues, particularly in the digestive system. An empty stomach can trigger gastric diseases like ulcers. Therefore, maintaining stomach health is crucial when fasting.
Eating at the wrong time or skipping meals will cause the stomach to increase gastric secretion, causing stomach damage and causing ulcers. Therefore, patients should pay attention to eating enough meals and on time.
Stomach ulcer symptoms usually worsen on an empty stomach and improve after eating. This is because food acts as a buffer, reducing irritation from stomach acids on the ulcer.
The main symptom of a stomach ulcer is a burning or gnawing pain in the abdomen’s centre. However, ulcers can also manifest as indigestion, heartburn, acid reflux, and nausea, which means they aren’t always painful.
The most common ulcer symptom is a dull or burning pain in your belly between your breastbone and belly button. This pain often happens around meals and might wake you up at night. It can last from a few minutes to a few hours.
Stomach ulcers, or sores on the stomach lining, occur due to reduced protective mucus and increased acid. Symptoms include burning stomach pain, particularly when the stomach is empty, along with dull pain, weight loss, nausea, vomiting, bloating, heartburn, and severe signs like bloody vomit.
Although the feeling of hunger and ulcer might seem alike, the difference is that hunger is stimulated by the Ghrelin hormone. In contrast, ulcer occurs when the lining of the stomach is eroded due to the presence of H. pylori bacteria and the excessive use of painkillers.
References
1. Engevik, A. C., & Hill, D. R. (2014). Gastrointestinal mucus and bicarbonate barrier: protection and repair. *Current Opinion in Gastroenterology*, 30(5), 511-518.
2. Pignatelli, B., Patsos, H., & Catalano, G. (2001). Gastric protection by prostaglandins. *Prostaglandins & Other Lipid Mediators*, 65(1-4), 93-99.
3. Sato, N., & Nagahara, A. (2012). Tight junction proteins and gastric ulcer healing. *Journal of Gastroenterology and Hepatology*, 27(Suppl 3), 103-110.
4. Wallace, J. L., & Sharkey, K. A. (1994). Pharmacotherapy of gastric acidity, peptic ulcers, and gastroesophageal reflux disease. In *Goodman & Gilman’s: The Pharmacological Basis of Therapeutics* (9th ed., pp. 901-915).
5. Lanza, F. L., Chan, F. K., & Quigley, E. M. (2009). Guidelines for prevention of NSAID-related ulcer complications. *The American Journal of Gastroenterology*, 104(3), 728-738.
6. Feldman, M., & Cryer, B. (1998). The importance of meal timing in the regulation of gastric acid secretion. *American Journal of Gastroenterology*, 93(3), 339-344.
7. Abadi, A. T. B., & Taghvaei, T. (2012). Probiotics, prebiotics and synbiotics: alternative strategies for the treatment of Helicobacter pylori infection. *Hepatitis Monthly*, 12(7), 100-107.

Chisom Maduechesi is a freelance health writer and researcher. She has a distinct passion for making quality health information available, making the slogan "Health is wealth" a reality for all. Chisom's areas of expertise include public health, nutrition and fitness.
We publish helpful posts every week!